|
Experimental
I. Acute Myocardial
ischemia – natural history
Summary
A large experimental study,
which required several years to complete, was designed (in cooperation
with Dr Adrian Kantrowitz, in his laboratory at Sinai Hospital in
Detroit) to evaluate the effects of intra-aortic balloon pumping
(IABP) on myocardial ischemia and resulting infarction. Experiments
were performed in anesthetized dogs, in which localized ischemia was
induced by ligation of coronary artery branch(es). In the initial
series of experiments, natural history of acute ischemia (behavior of
the ST segments and R waves) and infarct development (Q and R waves,
Q/R ratio) were studied with an array of 20 epicardial electrodes. As
previously accepted in similar studies, the epicardial extent of the
ischemic field was expressed as a number (N) of electrode sites
displaying ST segment shifts (NST), and its local “severity” by a sum
(E-sigma) of the magnitudes of ST segment elevations (EST) in
millivolts (mV) in the same area. In addition, Q wave development (NQ
and EQ), R wave behavior, and Q/R index were studied in acute and in
chronic experiments.
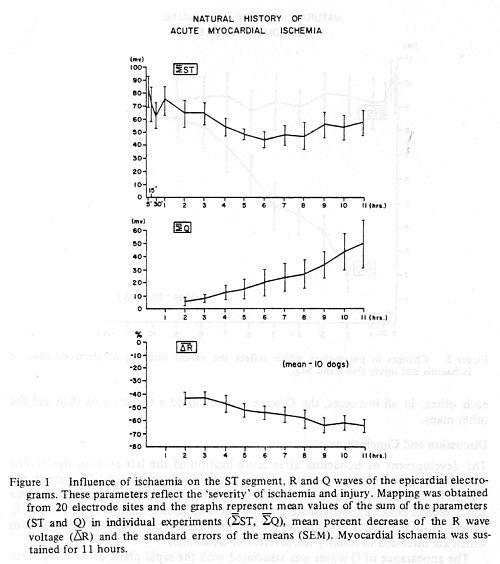
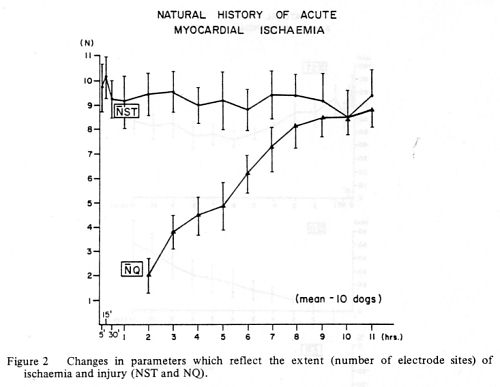
The maximum extent (NST) and
severity (EST) of ischemia at the sites with ST segment elevations was
seen usually already after 5 minutes. The area (NST) remained
essentially unchanged during the 11 hours of observation, but the sum
of ST segment elevations (EST) was gradually decreasing during the
first 6 hours and it was followed by a recurrent spontaneous slight
increase. Measurable Q waves (EQ) were seen after 2 hours and their
number (NQ) and depth were steadily increasing until the end of the
experiments. Development of Q waves was accompanied by progressive
reduction of the R wave voltage (ER). After 2 hours of ischemia,
approximately 20% of the electrode sites showed early Q wave
development and after about 9 hours, nearly all electrode sites with
initial ST segment elevations recorded the Q waves.
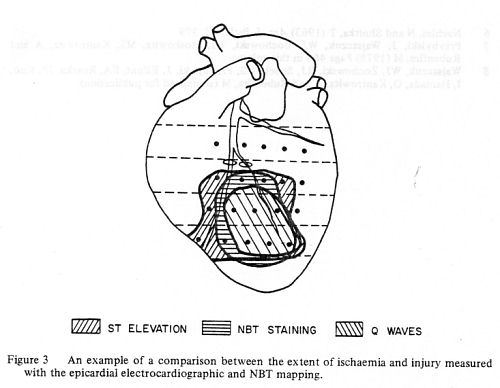
The extent of ischemia and
damage was further evaluated at the conclusion of the experiments by
gross pathologic studies with inspection, nitroblue tetrazolium (NBT)
staining and mapping and weighing of the damaged myocardium and with
light and electron microscopy.
The effects of IABP assistance
and reperfusion were noted in separate series of experiments. In
addition, the coincidental experimental interventions were observed
and their effect on the recording parameters were studied. Long-term
effects of myocardial ischemia and the extent of myocardial scarring
were evaluated in separate series of chronic experiments and are
described below.
(Natural
history of acute myocardial ischemia: electrocardiographic epicardial
mapping and nitroblue tetrazolium studies. Waldemar J. Wajszczuk,
Jacek Przybylski, Ryszard J. Zochowski, Edna A. Elfont, Joseph P.
Roszka and Melvyn Rubenfire. Progress in Electrocardiology. Edited
by Peter W. Macfarlane. Pitman Medical Publ. Co., Kent,
England, 1979, pp. 220-224.)
II. Acute Myocardial
ischemia – modifying factors
Summary
Natural
course of myocardial ischemia (or the parameters used for its
evaluation) can be occasionally modified by intended or unintended or
coincidental interventions. Knowledge of their effects on the
electrocardiographic manifestation of ischemia can prevent errors in
their interpretation.
Some of
them may be related to pharmacologic interventions and others to the
spontaneously occurring events such as extension of the zone and
severity of local ischemia or to alteration in systemic oxygenation.
Presented here are some of such circumstances encountered during our
experimental work and some of the examples of their effects on the
electrocardiographic recordings.
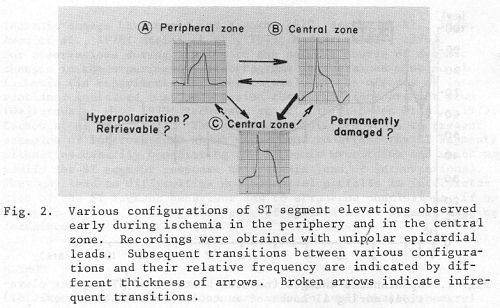
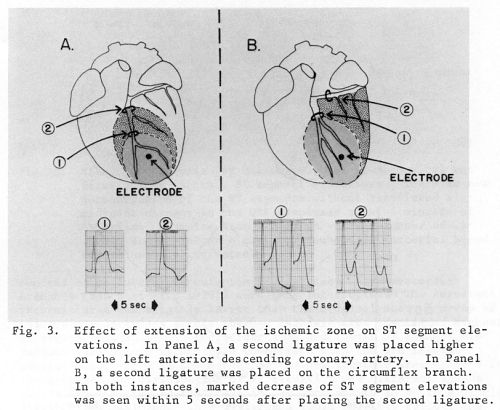
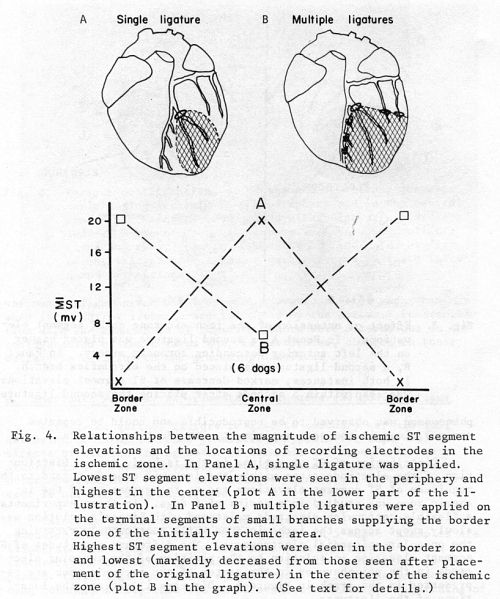
There
appeared to be different configurations of the ST segments in the
peripheral and central zones of ischemia – perhaps defining the zones
of reversible and irreversible ischemia. Extension of the ischemic
zone (by applying additional ligature on an adjacent coronary artery
branch) appeared to cause sudden decrease of the ST segment
elevation at the previously ischemic site(s) – (related to collateral
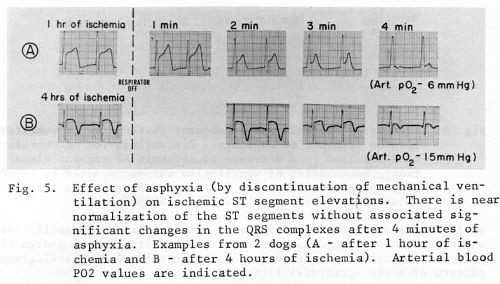
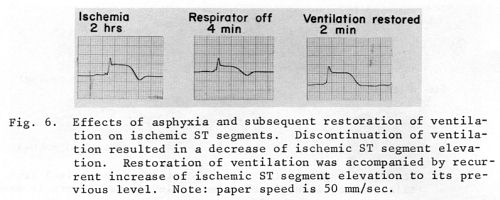
circulation?). Sudden changes in systemic oxygenation also
significantly affected the magnitude of ST segment elevations, leading
to their near-normalization in severe hypoxia (perhaps by equalizing
the oxygen gradient between the ischemic and previously normal
myocardium?). ST segment elevations increased again after improved
oxygenation and correction of the acid-base imbalance. Repeated
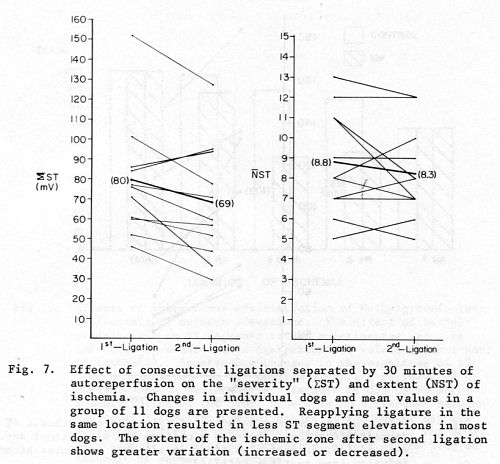
episodes of ischemia after a period of reperfusion caused usually
somewhat decreased manifestation (EST and NST) of ischemic parameters.
(In another group of chronic experiments (see below), it was noted
that the reperfusion-induced decrease of ST segment elevations was
associated with accelerated development of the Q waves).
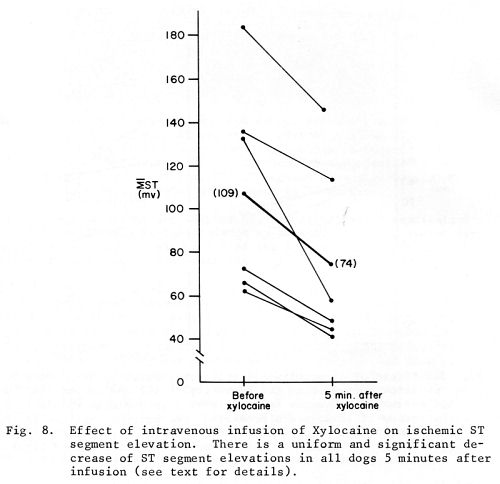
Effects of
administration of two medications was also observed. Marked decrease
of the ischemic ST segment elevation was seen 5 minutes after
intravenous bolus administration of Lidocaine and it persisted for
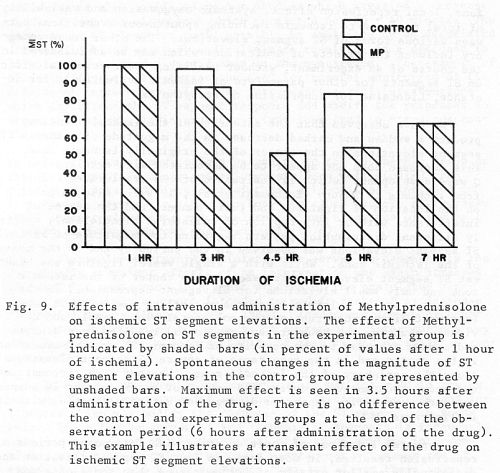
30-45 minutes. Slow intravenous infusion of methylprednisolone started
one hour after the onset of ischemia induced continuing decrease of
ischemic ST segment elevation, which was enhanced in comparison with
the spontaneously occurring ST segment changes, peaked aafter 3.5
hours and after 6 hours there was no difference between the treated
and control group
(Epicardial ST-segment mapping in acute myocardial ischemia. Examples
of coincidental experimental interventions which may affect
interpretation. Waldemar J. Wajszczuk, Jacek Przybylski,
Grzegorz Sedek, Ryszard Jacek Zochowski, Tadeusz Palko, Albert Whitty,
and Melvyn Rubenfire. Models and Measurements of the Cardiac
Electric Field. Edited by E. Schubert, Plenum Publishing Corporation,
1982, pp. 149-163.)
III.
Chronic myocardial ischemia and infarction
Summary
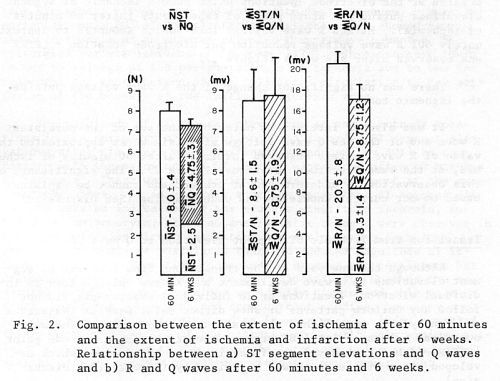
A separate
series of 10 experiments was devoted to study of the acute phase of
ischemia, after 60 min., and its comparison with the findings after 6
weeks. Acute phase recordings were performed under anesthesia during
limited thoracotomy and with minimized stress, the dogs were allowed
to recover and then chronic phase studies were performed after 6
weeks.
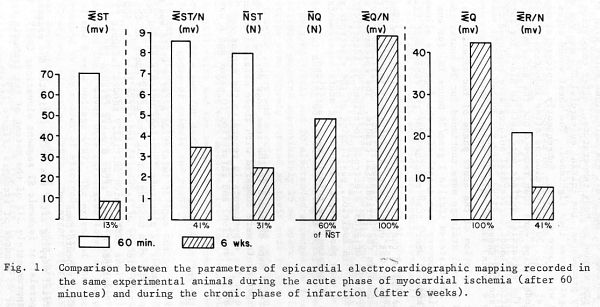
After 6
week, the extent of the epicardial zone with ischemic ST segment
elevations decreased by 69%; the magnitude of ST segment elevations
(at the sites with presumably persistent ischemia) decreased by 59%. Q
waves developed at 60% of the sites with earlier ischemic ST segment
elevations during the acute phase of the experiments; this was
associated with a 59% reduction of the R wave voltage.
A
different comparison revealed that, in the affected area after 6
weeks, the total area of ischemia (initial ST segment elevations) and
infarction (Q waves at 6 weeks) decreased by approximately 10%;
approximately 2/3 of the sites developed Q waves and 1/3 displayed
persistent (ischemic?) ST segment elevations; total QRS (R+Q) voltage
decreased by approximately 15%. The mean magnitude (in mV) of ST
segment elevations per recording site (EST/N) at 60 min. equaled
approximately the depth of the new Q waves (EQ/N) after 6 weeks. It
remains to be determined, whether the area of persistent ST segment
elevations represents a viable and recoverable myocardium or only a
potential arrhythmogenic hazard. Electron microscopic studies (see
below) revealed a fairly well preserved cellular ultrastracture in
these regions with only minimal cellular derangements.
(Natural
history of experimental myocardial ischemia. Observations in acute and
chronic studies. Waldemar J. Wajszczuk, Ryszard Jacek
Zochowski, Jacek Przybylski, Nicholas Z. Kerin, and Melvyn Rubenfire.
Models and Measurements of the Cardiac Electric Field. Edited by E.
Schubert, Plenum Publishing Corporation, 1982, pp. 165-173.)
|